Dr. Debasis Maity
Consultant Uro-Surgeon
Medical Discussion
Hematuria
Remember:
- Normal urine contains < 3 RBCs/HPF
- Microscopic hematuria =
> 3 RBC/HPFin urine. - Positive Dipstick for blood in urine indicates:
- Hematuria
- Haemoglobinuria
- Myoglobinuria
- M/C cause of hematuria is Acute Cystitis
Q. - M/C cause of glomerular hematuria is IgA Nephropathy
Q. - Papillary necrosisis is the cause of hematuria in Diabetics, Sickle cell disease, analgesic abuse, African Americans.
- M/C cause of milky/Cloudy urine is – Phosphaturia
Q. - M/C cause of painless hematuria after age of 50 yrs is – Bladder Cancer
Q - Pseudohematuria = Seen in ingestion of rifampicin, beet root, phenolpthaline.
Causes of Renal Papillary Necrosis
- Diabetes mellitus
- Pyelonephritis
- Urinary tract obstruction
- Analgesic abuse
- Sickle cell hemoglobinopathies
- Renal transplant rejection
- Cirrhosis of the liver
- Dehydration, hypoxia, and jaundice of infants
- Miscellaneous: Renal vein thrombosis, cryoglobulinemia, renal candidiasis, contrast media injection, amyloidosis, calyceal arteritis, necrotizing angiitis, rapidly progressive glomerulonephritis, hypotensive shock, acute pancreatitis
N.B.: Papillary Necrosis is not found in Renal Cell CarcinomaQ.
Differential Diagnosis of Coloured Urine
Cloudy/milky
- Phosphaturia (m/c)
- Pyuria
- Chyluria
Red
- Hematuria
- Hemoglobinuria/myoglobinuria
- Anthocyanin in beets and blackberries
- Chronic lead and mercury poisoning
- Phenolphthalein
- Phenothiazines
- Rifampin
Orange
- Dehydration
- Phenazopyridine (Pyridium)
- SulfasalazinE
Yellow
- Normal
- Phenacetin
- Riboflavin
- Bilirubin
Green-blue
- Biliverdin
- Indicanuria (tryptophan indole metabolites)
- Amitriptyline
- Indigo carmine
- Methylene blue
- IV promethazine (Phenergan)
- Resorcinol
- Triamterene (Dyrenium)
Brown
- Urobilinogen
- Porphyria
- Aloe, fava beans, and rhubarb
- Chloroquine and primaquine
- Furazolidone (Furoxone)
- Metronidazole (Flagyl)
- Nitrofurantoin (Furadantin)
- Brown-black Alcaptonuria (homogentisic acid)
- Hemorrhage
- Melanin
- Tyrosinosis (hydroxyphenylpyruvic acid)
- Cascara, senna (laxatives)
- Methocarbamol (Robaxin)
- Methyldopa (Aldomet)
- Sorbitol
Frequently Asked Questions:
- Etiology of hematuria.
- Differential diagnosis of hematuria.
- What is microscopic hematuria?
- Short notes : painless hematuria.
- Discuss the causes, investigations and management of a case of hematuria.
- A male patient aged 60 years attended surgical OPD with painless hematuria. How will you diagnose and treat the case?
Etiology:
-
Glomerular Hematuria ( = dysmorphic RBCs, RBC cast, and proteinuria)
- IgA nephropathy (Berger disease)
- Mesangioproliferative GN
- Focal segmental proliferative GN
- Familial nephritis (e.g., Alport syndrome)
- Membranous GN
- Mesangiocapillary GN
- Focal segmental sclerosis
- Unclassifiable
- Systemic lupus erythematosus
- Postinfectious GN
- Subacute bacterial endocarditis.
- Non – Glomerular Hematuria ( = circular RBC, no cast, proteinuria)
- Medical
- Tubulointerstitial disease
- Renovascular
- Systemic
- Drugs : Analgesics
- Anticoagulants
- Blood Dyscrasia
- Papillary necrosis
- Medullary Sponge Kidney
- PCKD
- Surgical
- Stone Disease
- UTI
- Urologic Tumors
- BPH
- CA Prostate
- Trauma
- Medical
Memoranda:
- Essential hematuria = Circular RBC, No Cast, No proteinuria
- Exercise induced hematuria:
- Occurs in long distance runners (>10kms)
- Noted at end of the run.
- Disappears with rest.
- Origin
- Renal – IgA nephropathy.
- Bladder – Bladder tumor.
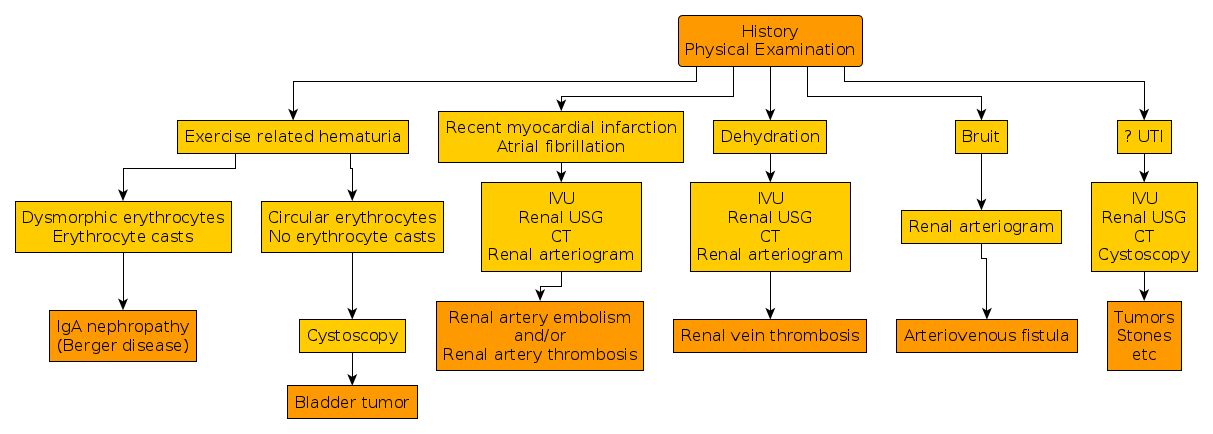
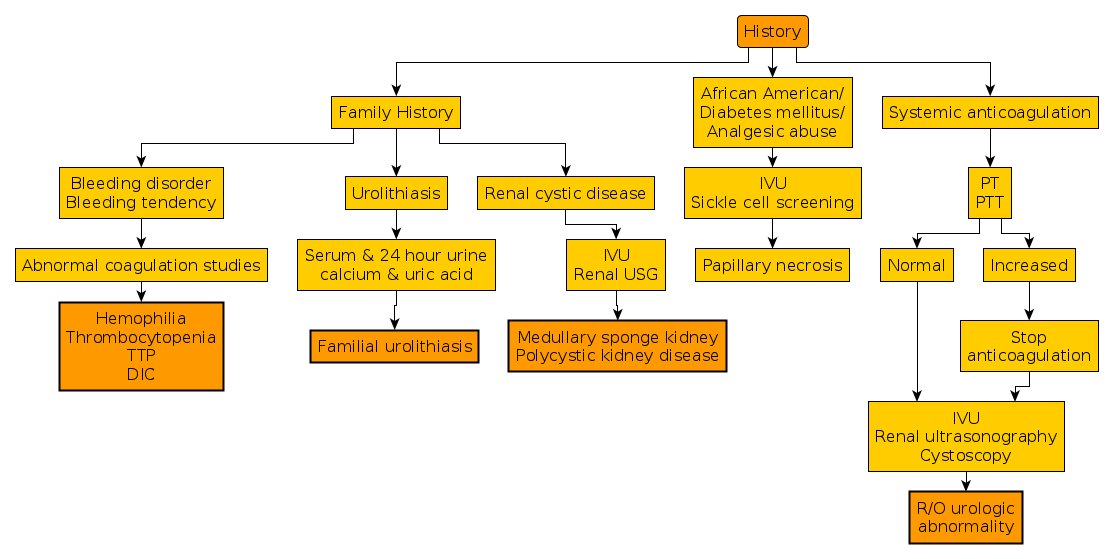
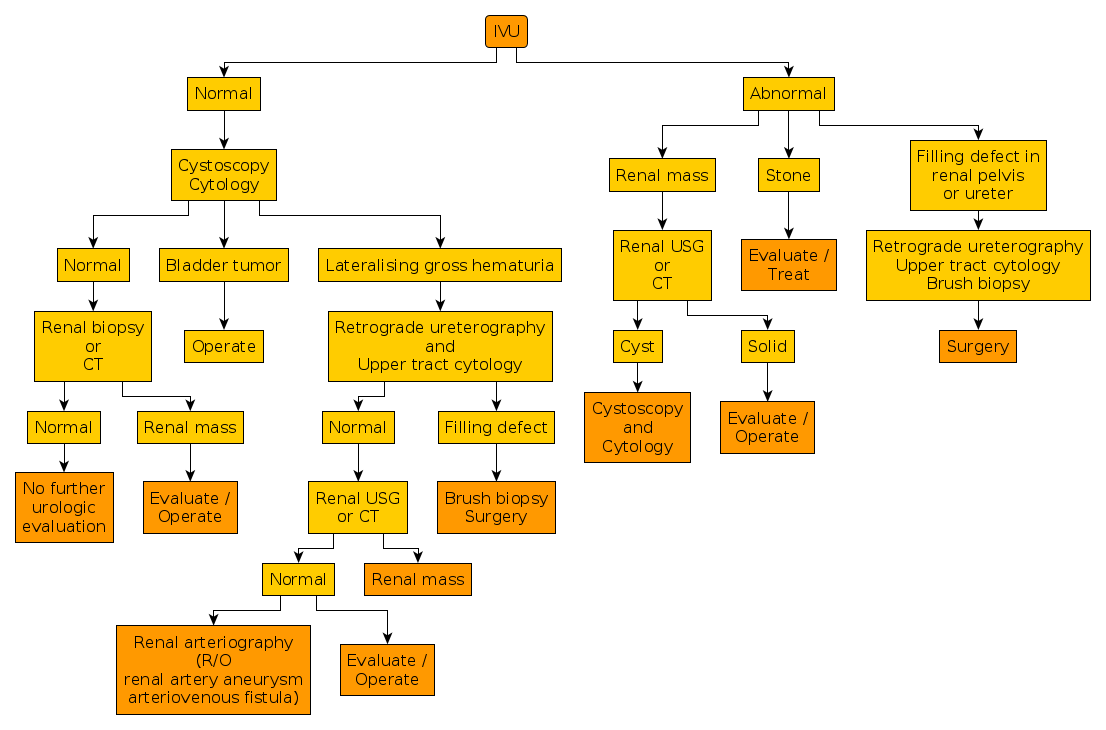
Approach:
In evaluating hematuria, following questions should be asked, and which help the subsequent diagnostic evaluation efficiently:
- Is the hematuria gross or microscopic?
- At what time during urination does the hematuria occur (beginning or end of stream or during entire stream)?
- Is the hematuria associated with pain?
- Is the patient passing clots?
- If the patient is passing clots, do the clots have a specific shape?
History
- H/O Trauma, drug intake.
- Timing:
- Initial hematuria
- from the urethra;
- least common,
- secondary to inflammation.
- Total hematuria
- most common
- from the bladder or upper urinary tracts
- Terminal hematuria
- secondary to inflammation in the bladder neck and prostatic urethra.
- Why terminal?
- Because the bladder neck contracts,squeezing out the last amount of urine.
- Initial hematuria
- H/O LUTS (hesitancy, urgency, frequency, nocturia, poor stream – indicate BOO/Prostatomegaly)
-
H/O associated pain
- With pain
- Stone
- Trauma
- without pain
- Tumor
N.B. Hematuria, is usually not painful unless it is associated with inflammation or obstruction.
- With pain
- H/O Gross/microscopic hematuria.
- H/O passage of clots
- Presence of Clots indicates a more significant degree of hematuria, and, accordingly, the probability of identifying significant urologic pathology increases.
- Shape of Clots
- Amorphous clots
- Origin: Bladder or prostatic urethra
- Vermiform(wormlike) clots
- Origin: Upper tract ( kidney & ureter )
- Amorphous clots
General survey
- Vitals: Pallor / BP / RR / HR / Temp / Urine output
Abdominal examination:
- Renal lump
- Palpable bladder
- Renal angle tenderness (Infective origin)
- Any bruise in the flank after trauma.
- DRE
- Evaluate prostatic condition.
Investigations
-
Urinalysis- pH (normal pH = 5.5 – 6.5):
- if alkaline indicates infection
- sterile pyuria in acidic urine
Q- Causes are TB, Stone, Malignancy, Interstitial nephritis, ↑IL-6 and IL-8.
- Culture: To detect uro-pathogens.
- pH (normal pH = 5.5 – 6.5):
-
USG of KUB Region:- Mainly to detect any
- Mass
- Hydronephrosis
- Prostatic volume
- Post void residual
- Any stone disease
- Mainly to detect any
Cystoscopy:- Cystoscopy should be performed as soon as possible, because frequently the source of bleeding can be readily identified.
- All patients with hematuria, except young women (<40 years) with acute bacterial hemorrhagic cystitis, should undergo urologic evaluation.
- Older women and men who present with hematuria and irritative voiding symptoms may have cystitis secondary to infection arising in a necrotic bladder tumor or, more commonly, flat carcinoma in situ of the bladder.