Dr. Debasis Maity
Consultant Uro-Surgeon
Medical Discussion
Dilemma in Diagnosis of CA Prostate
D-1) Persistently raised PSA and single negative prostate biopsy:
what next?
-
The first step is to assess adequacy of initial biopsy –
which depends on:
- No and location of biopsy cores taken, length of each core,quality of tissue sampled.
- Size of prostate (chance of finding any cancer is inversely related to prosate size).
-
what next = repeat biopsy.
but why?
- Detection rate on repeat biopsy will be 2 fold higher in an12 core extended biopsy scheme- (AUA 2012).
- Upto 30% improved detection rate on RPB (EAU-2013).
D-2) Role of new biochemical marker:
Aim is to reduce unnecessary Repeat biopsy.
-
NCCN guideline (EAU 2013)
%fPSA ( in pt with total PSA 4-10 ng/ml) Prostate Biopsy (PB) ≤10% Do PB .>10 - ≤25% Intermediate ≥25% No PB -
FDA approval
Progensa PCA3 assay
- what is this ?
- This is PCA3 score = ( PCA3 RNA/PSA RNA)
- Cut off value=25, in post DRE 1st catch urine. (some used-cut off=35)
- For whom?
- Male ≥50 yrs, one or more negative PBs, again highly suspicious for prostatic CA.
- why?
- CA detection rate 6% at PCA3 <5 to 57% at PCA3 >100.
- Sensitivity & specificity of PCA3 score of 35 are- 48% & 78% who underwent 10 core 2 sets repeat PB at 2 & 4 yr follow up.
- Superior than %fPSA.
- what is this ?
D-3) Dilemma if initial bx showed HGPIN (15-20%):
What next ?
- Single core
- No RPB
- Why?
- Because unrelated to Pca risk
- Multifocal
- RPB within 1 yr after initial bx
- “Delayed interval” PB every 3 yrs-( GODOY et al).
- Why?
- Because risk of CA on RPB - 40%
D-4) Dilemma if initial bx showed - ASAP (5%):
What next?
- RPB within 3-6 months
Why?
- Because 40% chance of cancer detection on RPB.
D-5) Dilemma in techniques / no of cores / sampling location during initial bx:
Sextant? / 10 cores? / 12 cores? / more?
Current recommendation:
-
10-12 core extended PB scheme, with additional cores from suspected area on DRE/TRUS is the most accepted method.
(some authors recommend adding a core from extreme apex on each side, because this is the m/c site where CA is missed during initial bx)
What is extended PB scheme?
sextant template + at least 4 & up to 8 laterally directed sampling from PZ.
Usually 12 cores.
Advantage?
Superior detection rate.
Vienna nomogram suggested (8-18) cores, based on pt age & gland volume, in PSA 2-10 ng/ml to ensure 90% certainty.
(for example= prostate size of 50-60 ml in pt <50yrs, 50s, 60s, 70s- 16, 14, 12 or 10 cores were prescribed respectively)
Most initial bx shown = further increase in no of bx core >12 has no significant benefit.
D-6) Repeat PB – what’s the optimal technique?
- Controversial.
- Recommendation is 10-12 cores extended bx, with additional core from suspected area by modern imaging.
Recently Scattoni et al developed some model,
| Pt with previous ASAP | Pt with %fPSA <10% | Pt with %fPSA>10% but no ASAP |
|---|---|---|
| 14 core without TZ sampling | 14 core bx with 4 TZ core | 20 core bx with 4 TZ core |
Algorithm for pt with prior negative biopsy (AUA updates 2012-1)
-
Assessing the adequacy of initial biopsy.
↓
-
F/T PSA is currently the most useful for predicting cancer on repeat biopsy.
(Newer marker such as PCA-3 and %(-2) proPSA are promising)
↓
-
Repeat bx include a minimum of 14 cores
(12 cores recommended for initial biopsy plus 2 additional core from right and left anterior apex)
(The yeild from transition zone is low)
↓
-
Fail to identify CA
↓
-
Saturation biopsy (>20 cores) is warranted
- After 2 negative saturation biopsy , finding of cancer is extremely low and if found, the significance of the cancer is questionable.
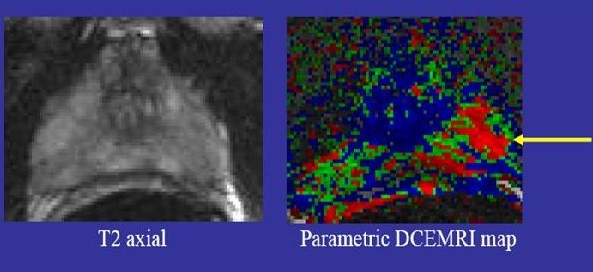
mp-MRI – (Multiparametric-MRI) for Prostate-malignancy
-
Includes T1 and T2 weighted sequences with at least 2 functional parameters–
-
dynamic contrast enhancement (DCE),
-
diffusion-weighted imaging (DWI),
-
apparent diffusion coefficient (ADC) mapping
- and magnetic resonance spectroscopy (MRS).
-
Q) Does mpMRI have a role in ruling-in and ruling-out clinically significant prostate cancer in men at risk prior to biopsy ?
-
MRI may rule out significant cancer and avoid a second biopsy series in case of persistent elevated PSA.
- There is clear evidence that targeting biopsies to areas suspicious for malignancy at mpMRI can reveal a greater volume of cancers and a higher grade than systematic 12-core biopsies.
Pt had high PSA & negative TRUS–bx. Later Cancer confirmed on MR-bx
MRI for the Detection, Localisation, and Characterisation of Prostate Cancer:
Recommendations from a European Consensus Meeting–
- Diffusion weighted MR (DW-MR) sequence is appropriate in detection of any cancer in PZ
- The Gleason grade of lesions in the PZ
- exclusion of clinically significant disease as defined by a lesion size ≥0.2 cm3 (approximately 7 mm) in PZ,
- exclusion of clinically significant disease as defined by a lesion size ≥0.5ml, in the PZ &
- exclusion of clinically significant cancer according to the definition of a lesion ≥0.5 cm3 and/or Gleason ≥4 + 3 in the PZ.
TRUS (Trans Rectal Ultrasonography):
- Uses:
- Biopsy
- Cancer Screening
- Prostate Gland Measurement and Calculation PSA Gland Density
- Advantages:
- Simple out-patient procedure
- Reasonably well tolerated
- Inexpensive
- Disadvantages:
- Low sensitivity, low PPV
- Large inter-observer variability
- Trans-rectal approach is irritable for some
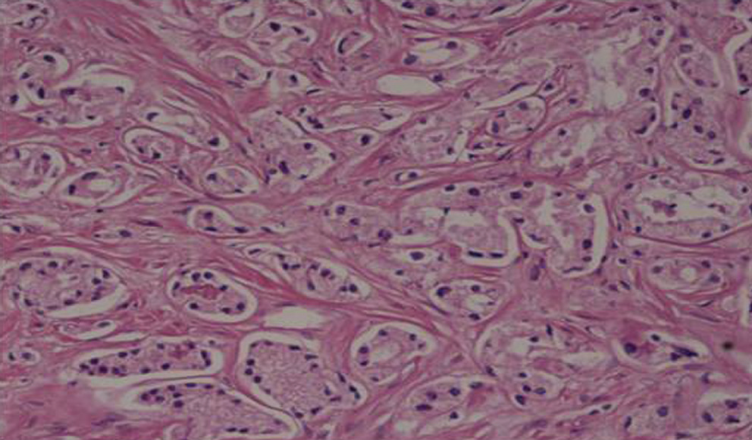
D-7) Diagnostic dilemma in histopathology report following robot assisted laparoscopic prostatectomy:
- There are reports in literature about the ‘vanishing cancer syndrome’ - the phenomenon of not finding any cancer in the radical prostatectomy specimen, despite a positive needle biopsy.
- This has important medico legal implications-
- Pt may feel that surgery has been performed unnecessarily or worse, still that cancer has been left behind in their body.
- Many benign conditions like Benign atrophy, post-atrophic hyperplasia, atypical adenomatous hyperplasia, seminal vesicle-type tissue, Cowper’s gland, and inflammatory processes like granulomatous prostatitis, xanthogranulomatous prostatitis and malakoplakia may be misinterpreted as adenocarcinoma in initial bx.
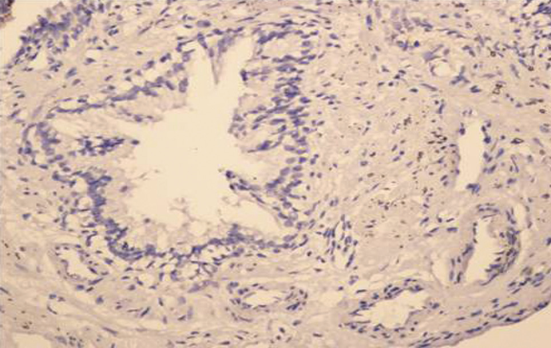
- In such cases use of immunohistochemical stains like p63, CAM 5.2, 34βE12 and AMACR may help in diagnosis.
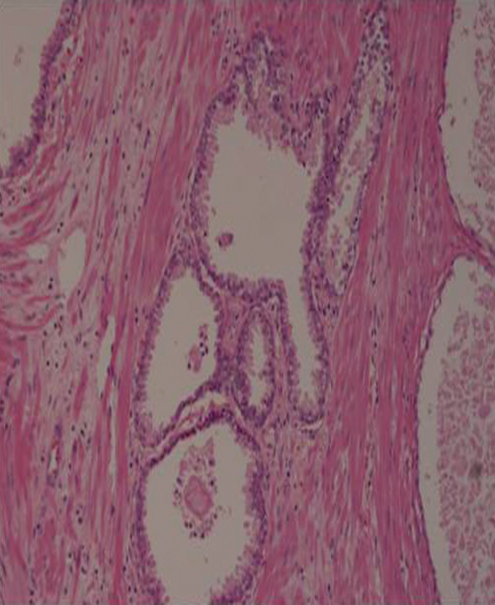
D-8)Diagnostic dilemma in histopathology report following radical prostatectomy:
TRUS biopsy showing adenocarcinoma prostate Gleason Score 3 + 3 = 6
BUT
Final histopathology slides of radical prostatectomy
specimen of same patient showing no tumor.
Negative AMACR staining